11/06/2024
Print PageDKTK Munich: Phagocytes from the culture dish for cancer therapy
Therapies using the patient's own immune cells, which have been armed against the cancer in the culture dish, have already proven to be very effective in some leukemias and lymphomas. For this purpose, the patient's T cells are genetically engineered with receptor molecules that specifically recognize certain characteristics of the tumour cells.
The problem, however, is that these so-called CAR T cells are unable to penetrate solid tumors efficiently, meaning that the therapies are usually ineffective. The solution could be another group of immune cells: certain phagocytes, so-called macrophages, which are part of the innate immune system.
Macrophages have the intrinsic ability to penetrate tumors. They can eliminate pathogens or diseased cells by engulfing them, and they also activate other lines of defense of the immune system. They can also be equipped with targeted receptor proteins against tumor characteristics - but: "Until now, it was impossible to grow phagocytes in the required quantity in the culture dish," explains Philipp Greif, head of a DKTK research group at the LMU Munich Hospital.
As soon as the blood stem cells, from which the phagocytes ultimately emerge, are isolated from their natural environment in the bone marrow, they begin to differentiate into mature blood cells. In this way, however, the "yield" of phagocytes remains too low to use them for medical applications.
A team led by Philipp Greif and Christian Wichmann, LMU Hospital, has now found a solution to this problem: The researchers genetically equipped human blood progenitor cells with the protein MLL-ENL. This abbreviation refers to the fusion of two proteins that together form a cancer-driving transcription factor that promotes cell division in many leukemias.
The DKTK researchers' trick: they equipped MLL-ENL with a controllable domain via which it can be activated with a chemical substance. Experts refer to this as an "inducible" transcription factor. If the blood stem cells were propagated in the culture dish in the presence of the substance, it was possible to grow large quantities of late monocytic blood progenitor cells, precursor stages of the macrophage. As soon as the substance was removed from the culture medium, the scientists were able to stimulate the cells to finally differentiate using suitable stimuli and immune messengers such as interferon-gamma - and they turned out to be functional macrophages.
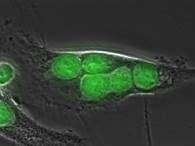
Analyses of the gene expression of the cells obtained in this way proved that they were extremely similar to natural monocytes, the precursors of macrophages. This was also confirmed by functional tests: the laboratory-induced phagocytes reacted to appropriate cytokines and eliminated bacteria and apoptotic cells.
Macrophages use their Fc receptors to recognize cells that have been marked as foreign by the immune system with antibodies. The phagocytes induced in the culture dish showed precisely this property: they were able to take up and eliminate foreign cells labeled with antibodies.
"Our induced phagocytes have the potential to destroy cancer cells in therapeutic applications by devouring them. The macrophages are to be equipped with a targeted receptor protein in order to direct them specifically against tumor cells. We will now test this option in further preclinical studies using a mouse model," explains Roland Windisch, first author of the current study.
"In this work, we have used inducible transcription factors for the first time to specifically produce large quantities of a certain cell type outside the body. By using other transcription factors, it may also be possible to use this principle to generate different types of blood cells for therapeutic applications in the culture dish," says Christian Wichmann, transfusion physician at LMU Hospital and head of the study. In this way, it may also be possible to produce various other human blood cells on a large scale and provide an alternative to blood donation in the future.
The project is funded by the Else Kröner-Fresenius Foundation (EKFS).