22/02/2018
Print PagePutting black skin cancer to sleep – for good
Cellular senescence – a state in which cells terminally cease to divide – prevents mutated cells from turning into tumors. This natural protective mechanism puts cells into a hibernation-like condition and is controlled by epigenetic tags located on the protein building blocks the DNA is wrapped around. These tags co-control how the genetic information encoded by the DNA is actually used. Cancer cells, however, were now found to deactivate the tags via a mechanism that was hitherto unknown.
An international team of researchers led by Professor Clemens A. Schmitt from Charité – Universitätsmedizin Berlin, the Max Delbrück Center for Molecular Medicine (MDC), and the Berlin Institute of Health (BIH) has now demonstrated that, in cancer cells, these important epigenetic marks are often erased by demethylase enzymes. Genetic or pharmacological inhibition of these enzymes restarts the protective mechanism, explains the team in an article published in the journal Cancer Cell*.
The research team conducted its study on almost 500 tissue samples taken from patients with black skin cancer, also known as melanoma. In roughly a third of the samples, researchers found a significant increase in the production of the demethylase enzymes able to stop the protective mechanism.
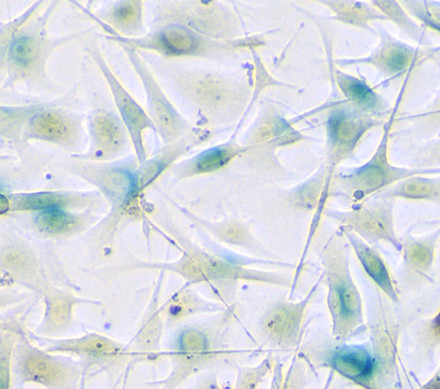
In melanoma cell cultures as well as mice and zebrafish with malignant melanoma, the researchers genetically modified the activity of these enzymes. They also used chemical agents to target and block them, which caused the cells to fall into the sleep-like state of senescence, thus stopping them to further divide. The experiment was even successful in mice with implanted human melanoma tissue, which is important information for future applications in patients. One of the agents used is currently explored in clinical trials for the treatment of lung and blood cancer.
In their investigation of melanoma samples from mice, the researchers observed that immune cells migrated into the tumor tissue once the senescence process had been reactivated by drugs. These and other important findings would not have been possible without using animal models.
Together with programmed cell death, cellular senescence is one of the body’s most important lines of defense against cancer. This protective mechanism epigenetically silences genes that regulate cell division. Methyltransferase enzymes mark histone proteins – the “spools” around which DNA is wrapped. These marks deactivate the section of DNA that is next to the histone. Clemens Schmitt and his team investigated two different demethylase enzymes that are able to counteract this process. Their ability to “erase” these histone marks makes the enzymes crucial for controlling and disabling senescence.
Cellular senescence is an important and welcome avenue for cancer therapies due to its ability to prevent the further growth of tumors. But its functions are not limited to blocking cancer, as Schmitt’s research team recently reported in the scientific journal Nature.
Clemens Schmitt believes the immigration of immune cells into the tumor that was observed in the senescence mechanism holds great potential for a new type of combination therapy. “We think the combined use of demethylase blockers and targeted immunotherapy might be extremely effective,” reports the clinical oncologist and researcher, who is Vice Director of the Division of Hematology, Oncology and Tumor Immunology in Charité’s Medical Department.
These findings are particularly promising for the treatment of melanoma, as this cancer responds poorly to chemotherapy and is better combated with the help of new immunotherapies. Schmitt and his colleagues now want to see how well immunotherapy and senescence-inducing therapy can be combined in clinical trials.
The study was supported by the German Research Foundation (Deutsche Forschungsgemeinschaft), the German Cancer Aid (Deutsche Krebshilfe) and the German Cancer Consortium (Deutsches Konsortium für Translationale Krebsforschung). Scientists from the Harvard Medical School in Boston, the Netherlands Cancer Institute in Amsterdam, the Weizmann Institute of Science near Tel Aviv, and the Imperial College in London collaborated in this work.
*Yong Yu et al. (2018): „Targeting the Senescence-Overriding Cooperative Activity of Structurally Unrelated H3K9 Demethylases in Melanoma.“ Cancer Cell 33. doi:10.1016/j.ccell.2018.01.002