31/05/2017
Print PageDKTK Essen/Düsseldorf: New findings support immunotherapy of skin cancer
Immunotherapy is today one of the most promising treatment methods for a number of skin cancers. Various immunotherapeutic approaches are also being used to treat Merkel cell carcinoma, a rare type of skin cancer that is particularly aggressive. However, only about 50 percent of the patients currently benefit from immunotherapy.
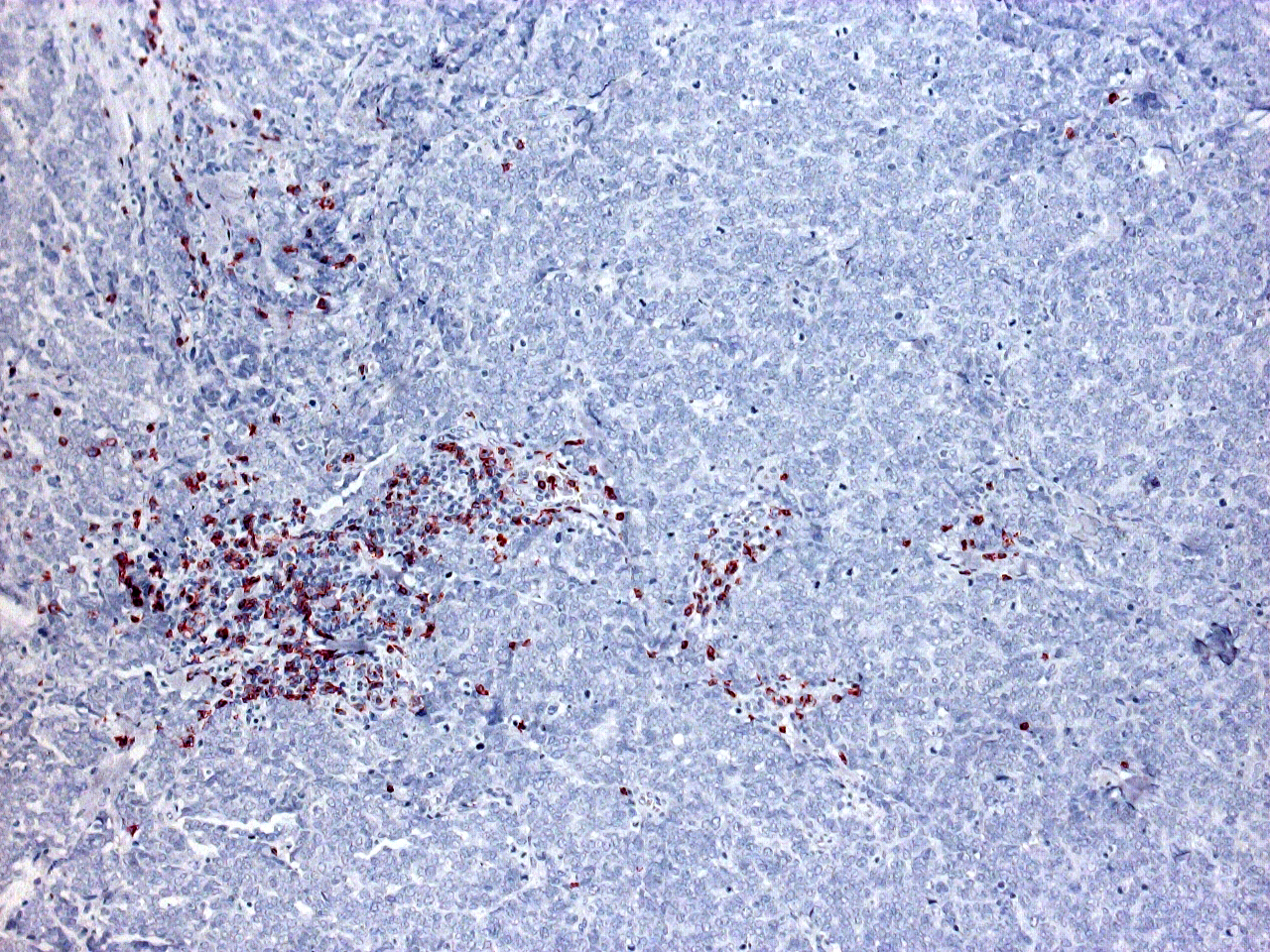
The cause for this is to be found in the molecular makeup of the immune system and in the way cancer cells manipulate it. In prior studies, scientists already noticed that in some patients Merkel cell tumors are overseen by the immune defense because they do no present human leukocyte antigens (HLA) on their cell surface. The HLA system plays a key role in humans for the process of labeling cancer cells for destruction by immune cells.
In the present study, scientists from the German Caner Consortium (DKTK) at Essen University Hospital have been the first to discover the mechanisms that the cancer cells use for their camouflage. The tumor uses so-called epigenetic mechanisms in order to silence genes that are essential for antigen presentation.
“The majority of Merkel cell carcinomas in Europe are caused by infection with the Merkel cell polyoma virus, which strongly manipulates the epigenetics of tumor cells,” said Professor Jürgen Becker, who is last author of the study and head of the DKTK working group “Translational Skin Cancer Research” at Essen University Hospital. “An important chemical label, the histone acetylation, is removed in the reprogrammed cancer cells. This leads to the silencing of various immune genes – a phenomenon that is also known as ‘epigenetic silencing’”. Genes that are involved in the presentation of tumor antigens on the surface of cancer cells are thus being silenced, and the immune system no longer recognizes the tumor cells.
In collaboration with colleagues from the University of Washington and Massachusetts General Hospital in Boston, the scientists have now found two methods to reverse this mechanism. One is to equip the cancer cells with the missing processed antigens. The cancer cells subsequently present them on their surface and are attacked and destroyed by T cells. In further experiments, the researchers blocked the key enzyme that is responsible for the inactivation, histone deacetylase (HDAC). As a result, the genes that are responsible for antigen presentation were reactivated and the tumor cell surfaces were loaded with more HLA again.
“Our results show that the camouflage in Merkel cell carcinoma can be reversed pharmacologically,” said Becker, a physician. He is confident that the new findings will improve clinical outcomes of immunotherapies to treat this type of skin cancer. “First we will test the effectiveness of various combination therapies with clinically applicable HDAC inhibitors. The next goal is to conduct clinical trials with patients for whom immunotherapeutic approaches have been ineffective until now.”
Reference
Cathrin Ritter et al.: Epigenetic priming restores the HLA class-I antigen processing machinery expression in Merkel cell carcinoma. In: Scientific Reports 2017,
doi:10.1038/s41598-017-02608-0 http://www.nature.com/articles/s41598-017-02608-0