04/02/2021
Print PageA defect with serious consequences: Epigenetic reprogramming turns neural stem cells into drivers of childhood brain tumors
The Hopp Children’s Cancer Center Heidelberg (KiTZ) is a joint institution of the German Cancer Research Center (DKFZ), University Hospital Heidelberg (UKHD) and the University of Heidelberg (Uni HD).
The abbreviation DIPG stands for diffuse intrinsic pontine glioma (brain stem glioma) and describes a rare type of childhood brain tumor for which there is currently no cure or life-improving treatment. Brain stem gliomas grow fast and aggressively and can spread rapidly as a result of cell migration in the brain. “The situation for patients with brain stem gliomas is still very depressing,” says KiTZ Director Stefan Pfister, who is head of the Pediatric Neuro-Oncology Department at the DKFZ and works as a consultant at University Hospital Heidelberg (UKHD). “Standard therapies such as radiotherapy and chemotherapy are not effective in these patients in the long term, and the average survival time following diagnosis is sadly just around 9 months.”
A discovery made a few years ago, however, may offer a route to new treatment methods: nearly 80 percent of patients were found to share the same genetic defect. In these patients, histone H3.3, a protein that is responsible for packing our DNA in the cell nucleus and for switching genes on and off throughout the genome, is mutated in the tumor genome: the amino acid lysine (K) is replaced by a methionine (M) at position 27 of the amino acid sequence. This is known as a K27M mutation.
This exchange has serious consequences for childhood brain development: K27 methylation in stem cells is an important epigenetic signal for turning them into healthy nerve cells. But methyl groups cannot attach to methionine. If this important signal is missing, gene regulation spirals out of control and important development genes are activated at the wrong time, including some that can promote the development of tumors.
But at what point, or in which type of precursor cell, in childhood brain development does the gene defect cause tumors to develop? And how can this process be influenced? “In young patients, the tumors only occur in a particular development time frame,” explains lead author Daniel Haag, who works at the KiTZ and at Stanford University in California. “This is why we investigated the consequences of the mutation in various precursors of nerve cells and supporting cells in the brain, so that we could identify a potentially critical cellular development window for tumor formation.”
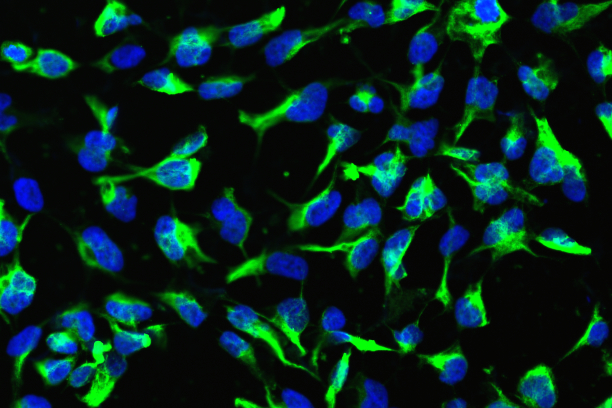
The study found that in induced pluripotent stem cells (iPSCs), which do not yet have the potential to develop into any kind of body cell, the absence of the methylation signal at K27 was so fatal that they did not survive the defect. By contrast, the researchers observed increased cell division in cells that had already differentiated into neural stem cells (NSCs) or precursor supporting cells in the brain.
The team was then able to show that the H3K27M mutation does actually lead to the onset of brain stem gliomas, and identified the underlying mechanisms in a laboratory model: mice with human neural stem cells, in which the K27M mutation could be selectively activated, developed malignant brain stem gliomas after 20–30 weeks. However the tumors only developed if the tumor suppressor protein TP53 had been genetically switched off at the same time. Neither the absence of TP53 on its own, nor the H3K72M mutation alone had this effect. In more differentiated precursor cells, however, the mutation did not cause tumor growth.
In neural stem cells, the K27M mutation also caused several genes that are important for brain development to be activated earlier than usual, including genes responsible for the growth of later precursor cells. “The absence of H3K27 methylation appears to have a drastic effect on neural stem cells, blocking the cellular development program and reprogramming them, as shown in our epigenetic analyses,” says Daniel Haag. “On the one hand, the cells retain their status as stem cells with the ability to self-renew, while at the same time a genetic program is activated, similar to that activated in late precursor cells, which triggers cell division. This turns them into aggressive tumor cells.”
The scientists therefore assume that early neural precursor cells represent the key stage for the development of brain stem gliomas. “For the first time, thanks to these new findings, we have a suitable test system that we can use to investigate the efficacy of new therapy concepts to combat this terrible disease,” says Stefan Pfister.
Original publication: D. Haag et al. The H3.3K27M Mutation Drives Neural Stem Cell-Specific Gliomagenesis in a Human iPSC-Derived Model. In: Cancer Cell (Online publication 4th of February 2021). DOI: 10.1016/j.ccell.2021.01.005.