08/06/2016
Print PageDKTK München: Putting a brake on leukemia cells
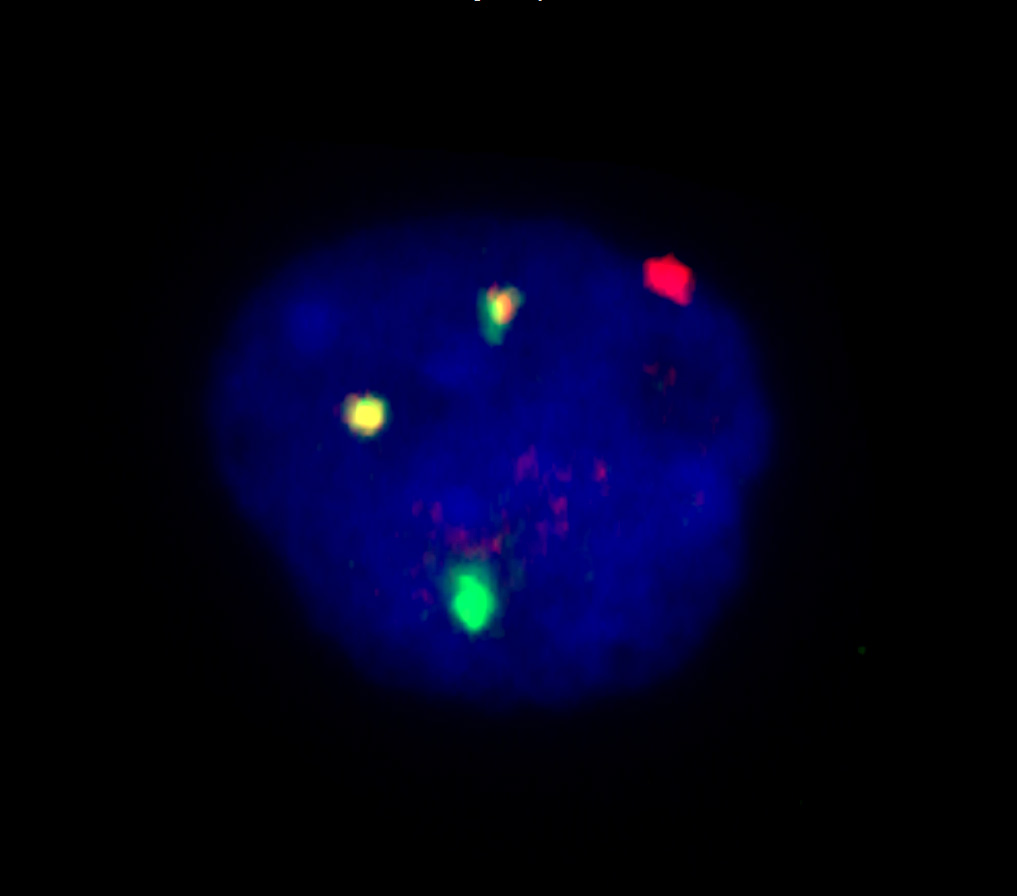
Biomarkers play an important role in modern cancer medicine. They are used as tools to diagnose cancers more precisely and to better predict the course of the disease. One marker that is frequently associated with leukemia is a chromosomal abnormality called t(8;21) translocation, in which a part of chromosome 8 connects with chromosome 21. Back in the 1970s, researchers already recognized that in a substantial percentage of patients suffering from acute myeloid leukemia (AML), the transformed cells exhibited this chromosomal abnormality. However, scientific studies also showed that the chromosomal rearrangement alone is not sufficient to cause leukemia.
In a research project as part of the German Cancer Consortium (DKTK), researchers at the Department of Internal Medicine 3, Munich University Hospital (LMU), have now discovered a new mutation that promotes the growth of cancer cells. The mutation in the ZBTB7A gene boosts the energy metabolism in the cells. “In healthy cells, the active ZBTB7A gene acts like a parking brake on metabolism,” said Philipp Greif, who leads the DKTK Junior Research Group “Pathogenesis of Acute Myeloid Leukemia” at LMU. “If the gene is defective, cancer cells get more energy to use for proliferation.”
Higher ZBTB7A gene activity correlates with a better chance of survival
Reversely, the scientists were able to show that the growth rate of leukemia cells can be reduced by genetically modifying the cancer cells in such a way that they produce higher levels of active ZBTB7A. The investigators also observed an indication of the gene's growth-inhibiting effect in the clinic: Leukemia patients in whose cancer cells the gene was transcribed at higher levels had significantly better chances of survival than patients in whom the gene was hardly active or not active at all.
Philipp Greif is one of the clinical researchers at the DKTK who are trying to find new, more targeted approaches in the treatment of cancer patients. “Assessing the course of the disease using genetic markers helps us recommend the right therapy,” Greif said. “In some cases, the leukemia may be curable with chemotherapy alone, while in others, subsequent stem cell transplantation is the only chance for the patients to be cured.” Using the available sample material at the LMU Laboratory for Leukemia Diagnostics and the collections at the other DKTK sites, the scientists now plan to explore whether the new marker can be used to customize therapies for individual patients.
Starving the leukemia cells
The discovery is also a promising starting point for developing new approaches toward treating AML patients. “It might be possible to use specially modified glucose molecules to block the energy production process in AML cells,” said Luise Hartmann, who is the first author of the study. “Initial clinical trials in other cancers have already shown that these agents are well tolerated by patients”.
About a quarter of all leukemia patients with the t(8;21) chromosomal abnormality display the mutated ZBTB7A gene. But the scientists also observed a clear link between the gene’s activity and the course of the disease in leukemia patients in whose cancer cells no mutations in the ZBTB7A gene were detected. “Therapy with the metabolic inhibitor might therefore work in a wider circle of patients,” Greif said. This approach might also become interesting for other types of cancer. ZBTB7A mutations also occur in other cancers, such as in gut cancer.
Original Publication:
Hartmann, L. et. al.: ZBTB7A mutations in acute myeloid leukaemia with t(8;21) translocation. In: Nature Communications (2 June 2016). DOI:10.1038/ncomms11733