01/12/2016
Print PageDKTK Tübingen: €2.5 million for developing a novel cancer immunotherapy
In the German Cancer Consortium (DKTK), the German Cancer Research Center (DKFZ) in Heidelberg joins up as a core center in long-term collaborations with university institutes and hospitals all over Germany that are specialized in research and treatment with a focus on oncology.
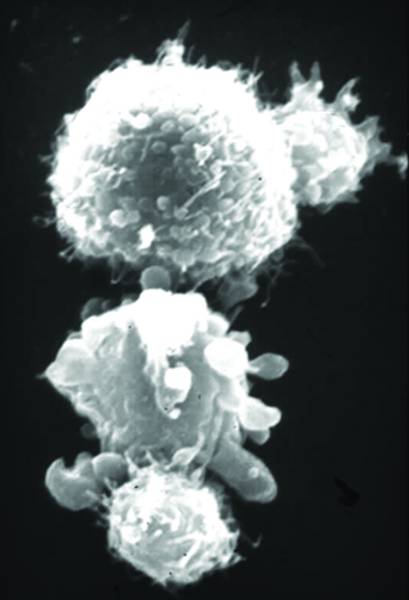
It is an intriguing idea: Antibodies with two different binding sites attach with one of their “arms” to a tumor-specific molecule on cancer cells. With the other arm, they attach to a protein that is responsible for activating immune cells. In this way, they establish contact between cancer cells and immune cells, thus enabling the immune system to attack the tumor.
Helmut Salih and Gundram Jung, two researchers working at the DKTK partner site at Tübingen University Hospital, have developed a “bispecific” antibody of this type. They combined parts of an antibody against the prostate-specific protein PSMA with binding sites for a T-cell molecule called CD3. The binding to CD3 activates the T cell to attack. PSMA, the prostate specific membrane antigen, is produced by prostate cancer cells. In addition, it is found on squamous cell carcinomas such as in the lungs, the skin and tumors of the head and neck as well as on the tumor blood vessels of other cancer types.
Salih and Jung used genetic engineering to develop a bispecific antibody called CC-1, which has a number of favorable characteristics: It leads to immune attacks both against the cancer cells and the blood vessels of the tumors. This increases the effectiveness of cancer immunotherapy compared to previous approaches. Additionally, the antibody is comparatively stable, remaining active in the bloodstream for a long time after the infusion. This makes treatment easier. The antibody has also been selected with a view to reducing expected undesired side effects of the treatment as much as possible.
This is where the funding from the Helmholtz validation fund comes in. The money will enable the researchers to execute the next steps in the pharmaceutical development of the antibody independently and rapidly, thus preparing their findings as swiftly as possible to be applied for patients.
Salih and Jung will now use the €2.5 million to finance the next steps that are required in the drug development process: CC-1 must be manufactured in sufficient quantities in clinical quality under the so-called GMP regulations. Laborious toxicological examinations are required to make sure that the antibody does not cause any undesired reactions. And finally, the researchers plan to conduct a first clinical trial with 20 participants that will involve several DKTK partner sites.
“The Helmholtz funds will enable us to execute the remaining preclinical steps and to show first evidence of efficacy in a clinical trial. This is usually not possible for an academic institution without substantial participation of the pharmaceutical industry,” Salih said. “Once these steps have been successfully concluded, our antibody can rapidly be developed to marketability jointly with a partner. In this way, we hope to be able to make a promising and urgently needed therapy option available for patients much more quickly.”